 (212) 861-9797
Book an Appointment
(212) 861-9797
Book an Appointment
 (212) 861-9797
Book an Appointment
(212) 861-9797
Book an Appointment
Of Combined Eye Surgery Experience
Eye Procedures Completed
Lectures Nationally & Internationally
From the moment you enter the office you are treated with respect from all the staff. The office operates efficiently to ensure that all patients have the time to be seen and talk with their physicians. I am very pleased with the care. Compassion and overall kindness that has been shown to me.
I have been seeing Dr. Engelbert for several years. He is smart, compassionate, and skilled. He has maintained the quality of my vision, and I consider myself extremely lucky to have been referred to him for my care.I recommend him without reservation.
I have been seeing Dr. Engelbert for several years. He is smart, compassionate, and skilled. He has maintained the quality of my vision, and I consider myself extremely lucky to have been referred to him for my care.I recommend him without reservation.
Our internationally-renowned ophthalmologists and Retinal Detachment specialists have trained and taught at some of the finest and most respected academic institutions in the world. As leading eye doctors and the best-rated Retinal Detachment specialists, they have devoted their time and resources to research and the development of new diagnostic and therapeutic strategies. This exceptional and unique expertise, joined with their attentive, empathetic concern and careful approach means that even expert ophthalmologists turn to VRMNY doctors first when they or their families need care.












The retina can be likened to film in a camera. It is the light sensitive structure that lines the back of the eye. The part directly in the back of the eye is the macular region. Because of the structure of the macula and the cells that are there, the macula supplies sharp vision and provides most of the color information being sent back to our brains.
The rest of the retina supplies a lower resolution image that gives us the wide field of view we ordinarily have. This side vision is very important in functioning in the modern world. The retina is not connected to the back of the eye in a firm way. Under some circumstances the retina can pull away from the back of the eye. Since the retina gets much of its oxygen and nutrition from the tissue in the back of the eye, this can lead to significant harm to vision.
The center of the eye is filled with a jello-like substance that is called the vitreous. When we are young, it is completely homogeneous and attached to the retina that lines the inside of the eye ball. As we get older, the vitreous shrinks, and parts of it become more stringy, others more liquid. This causes the slow increase in floaters over the course of our lives. However, when the shrinking vitreous eventually pulls away from its attachments to the retina, it may cause tears at points of particularly firm attachments. The pulling away of the vitreous causes the retina to send flash signals to the brain. If the retina is torn, there is often bleeding into vitreous, leading to a sudden and often dramatic increase in floaters. This is rare before the age of 40, but by the age of 70, 70% of people will have experienced a vitreous separation, or vitreous detachment (PVD) – not to be confused with a retinal detachment.
Most PVDs do not lead to a detachment, but it is important to be examined once flashes and/or floaters are noticed. If there is a retinal tear, it can usually be taken care of with an in-office laser procedure, and a retinal detachment prevented.
If untreated, retinal tears may progress to a retinal detachment, which is usually more involved to repair. This most common type of detachment that is called a “rhegmatogenous” retinal detachment.
An in-office laser procedure can be performed, where a contact lens is placed on the eye, and a laser beam directed onto the retina to surround the retinal tear with light laser burns. This leads to a permanent adhesion of the retina to the eye wall within a matter of a week. This is about 90% effective in preventing a retinal detachment.
If the detachment is very limited in extent it may be possible to treat it by applying laser burns around it and prevent the detachment from becoming larger.
Often, there is significant bleeding associated with a retinal tear. Usually, the bleeding gets absorbed over time, but if the vision remains poor because of the blood in the eye, it may be helpful to perform a vitrectomy to remove the blood and replace it with clear fluid, thus restoring clear vision.
If there is a more than localized retinal detachment, surgical repair is usually indicated.
There are several different ways the retina can detach from the back of the eye.
Most commonly, a tear in the retina allows fluid from the vitreous cavity under the retina, and slowly separates it from the eye wall.
It can also be pulled by force from the eye wall. There is no hole or tear in the retina, just brute force. Furthermore, an excessive amount of fluid produced under the retina by disease may float the retina away from the back of the eye.
“Rhegmatogenous detachment” is the fancy name for a retinal detachment that results from one or more retinal tears allowing fluid from the center of the eye to pass under the retina. This is the most common form of a retinal detachment. This usually occurs in middle-aged or older people when their vitreous separates.
Some diseases, such as diabetes, cause blood vessels and cells similar to those found in scar tissue to grow from the retina into the jello-like center part of the eye. This center part is called the vitreous. At first these blood vessel stalks look like treed or fans of seaweed. They are prone to bleed. Bleeding commonly leads to more scar tissue. Contraction of the scar tissue can pull the retina away from the back of the eye.
Several different conditions can lead to the same endpoint. For example, long-standing retinal detachments may lead to scarring, which can make reattachment by surgery more involved.
A complicated net of blood vessels exists under the retina in a structure called the choroid. The retina has the highest need for oxygen in the body per gram of tissue. If the retina had enough blood vessels to supply this requirement we would have a difficult time seeing because of all the blood vessels. Instead the eye has a nice design feature. A dense network of blood vessels delivers oxygen to the retina from below. This layer is called the choroid, and the choroid has the highest blood flow per gram of tissue in the body. Problems can arise if the vessels in the choroid become excessively leaky. If you have ever injured your elbow or knee you know the joint can become swollen. The swelling is from fluid leaking from blood vessels. Imagine the choroid – if that becomes inflamed there are many vessels that could leak. Fluid produced in the choroid will make that layer swollen, but the fluid oozes up under the retina and accumulates there. In exudative detachments the retina is floats off of the back of the eye.
While retinal detachments in young people are less common, they can happen for several reasons. Vitreous separation (PVD) usually occurs later in life, but can happen prematurely in younger people, for example if they are very near-sighted, or have experienced trauma to the eye.
Also, very near-sighted patients often have peripheral lattice degeneration, which can harbor small full-thickness defects that can slowly allow fluid under the retina. In contrast to retinal detachments from retinal tears in the context of a PVD in older people, flashes and floaters are rarely perceived by these patients. The detachment may progress very slowly and remain unnoticed until it starts to affect the central vision.
Also, exudative detachments may occur in young patients, for example pregnant women with preeclampsia, or patients with certain inflammatory conditions of the eye that affect younger individuals.
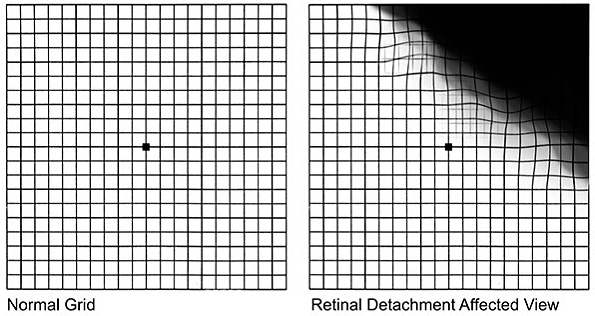
The most common symptoms of a retinal detachment include:
Diagnostic Testing

The principle way doctors at VRM diagnose a retinal detachment is through direct examination of the eye. This can help identify which of the three types of causes for retinal detachment is the problem. Additional testing might be required. Ultrasound is used to evaluate the position of the retina and to look at deeper structures in the eye. Optical coherence tomography (OCT) provides cross-sectional information about the retina and choroid, the nourishing blood vessel layer underneath the retina. Fluorescein angiography may be helpful in grading the amount of leakage in exudative detachments, as well as clarify the source for the leakage. As in other fields of medicine diagnostic testing helps establish the diagnosis, the mechanism of disease, serves to document disease severity, may direct treatment, and helps in monitoring disease progression.
Each form of retinal detachment has a different cause, and to repair the detachment the root causes need to be addressed.
Fixing detachments from a retinal tear
A retinal tear leading to a detachment requires closing the retinal defect for the detachment to be repaired. When retinal doctors talk about closing a retinal defect, what they mean is that the flow of fluid through the retinal tear to the space under the retina must be blocked.
The vitreous and any pulling by the vitreous on a tear is removed from the eye with small instruments under an operating microscope. The fluid under the retina is sucked out and laser welds are put around the tear or hole to seal the defect so no new fluid can come under the retina. The eye is usually filled with gas to hold the retina in place until the welds become strong, which takes about a week. Sometimes a thick fluid, silicone oil, is used instead of gas. The advantage of vitrectomy is that the doctor can directly see the defect and pulling if present and fix the problem. The disadvantage of vitrectomy is that the gas bubble used to hold the retina in place does not work well if the defects in the retina are at the bottom of the eye because the gas bubbles rise. Patients cannot see well if their eye has gas, and usually have to position with the face looking down for a certain amount of time. Cataracts are common after vitrectomy surgery. This type of eye surgery is generally done in a hospital setting.
Instead of removing the traction pulling from the inside of the eye, the outside wall of the eye can be indented toward the traction to relieve the force on the retina. To achieve this a piece of silicone (scleral buckle) is sewn on the outer wall of the eye (sclera). A freezing probe is often used to make welds between the retina and back wall of the eye. The advantages of scleral buckles are that they do not involve operating on the inside of the eye and that broad areas of the retinal periphery can be supported by the buckle. Often times, intraocular gas and the necessity to position face down after surgery can thus be avoided.
Scleral buckle eye surgery is generally done in a hospital setting.
A gas bubble can be used to seal a retinal tear. In pneumatic retinopexy a gas bubble is injected into the eye and the patient’s head is positioned to put the gas bubble over the tear. In many patients the fluid under the retina will be cleared by the body and laser welds will prevent any new fluid from coming through the tear. A freezing probe can also be used to make welds. The advantages of pneumatic retinopexy are that it is a quick in-office procedure that is minimally invasive. The disadvantages are that not all types of retinal tears can be repaired and the success rate overall is lower than for vitrectomy and scleral buckling
In most cases of traction retinal detachment a vitrectomy is performed. A vitrectomy is performed, and the vitreous as well as scar tissue that is pulling on the retina is removed from the surface of the retina with tiny forceps. If there are retinal defects, they are lasered as in “simple” rhegmatogenous retinal detachments. Unless there are not retinal tears, the eye is filled with gas or oil to hold the retina in place until the laser weld has created a permanent adhesion.
Successively putting the retina back into place is common after surgery. The success rate of the retinal detachment surgery depends on the mix of cases examined in any one study, but for most studies the proportion is about 90%. Of the failures most can be eventually repaired with an additional surgery. The amount of visual acuity return after surgery depends on the amount of damage occurring before the surgery. Detachment of the macula leads to damage and loss of vision depending on the extent and duration of the detachment.
There are two main causes for failure in cases of retinal detachment surgery.
The first is that the body may make scar tissue in the eye. This scar tissue grows on the retina and also in the vitreous cavity. After a while the scar tissue shrinks and pulls the retina in toward the center of the eye. This form of scar tissue has a special name, proliferative vitreoretinopathy.
Fortunately scar tissue leading to redetachment is not that common and repeat surgery if it does occur is often successful.
The second main reason to have another detachment is a repeat of what caused the detachment in the first place. A second tear can form in the eye leading to another detachment. This will require additional surgery. It is often not possible to know if and when a second tear will form.
If the tear is detected early, laser treatment to make welds can prevent progression of a detachment in many patients. The symptoms of retinal tears are not necessarily that different from that those experienced by patients having a simple vitreous separation.
If you have new or sudden flashes or floaters, darkness over part of your visual field, or a new loss of vision that does not go away, call your eye doctor or ophthalmologist right away. Floaters and flashes may be warning signs of retinal detachment.
There is no way to tell over the telephone if there are just simple floaters or a retinal tear. That is why examination by a doctor at our Retina Vitreous Centeris necessary. If there is no retinal tear, well that was just a false alarm. If a retinal tear is present, then a ‘whole lotta hurt’ potentially could be saved by an in-office laser procedure.